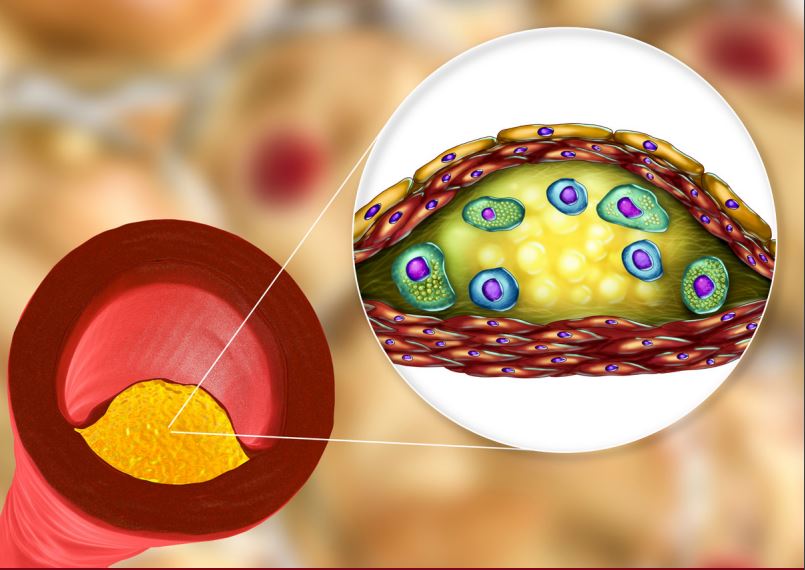
Residual Risk: Beyond LDL-C Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of death in the United States, and its prevention and treatment continue to be an area of utmost importance.1 Elevated low-density lipoprotein cholesterol (LDL-C) is a well-established ASCVD risk factor and significant advances have been made to lower it by using established and new strategies, including statin therapy, ezetimibe, and PCSK9 inhibitors.2,3 However, while lowering LDL cholesterol (LDL-C) remains central in the prevention and treatment of ASCVD, residual risk may be present even after the optimization of LDL-C levels.4
Current therapies that primarily target LDL-C may not address other drivers of atherosclerosis, including triglycerides (TGs), which seem to be part of the causal pathway in high-risk patients.2 In certain high-risk patients, including those with pre-existing ASCVD, or that have type 2 diabetes and/or metabolic syndrome, intensive treatment with statins and newer therapies to lower LDL-C may not address the full spectrum of cardiovascular prevention.4 In these patients, the interplay between phenotypes that promote both a proinflammatory state and atherogenic dyslipidemia (including elevated TG levels), requires additional measures to optimize both primary and secondary ASCVD prevention.2,4